
Here is how it’s explained based on data from StuffThatWorks:
Up to 15% percent of women between the ages of 18-45 suffer from Polycystic ovary syndrome (PCOS), yet it is estimated that it takes, on average, up to three visits with health professionals over the course of 2-3 years to be accurately diagnosed. Why? That’s what we’re trying to figure out. By analyzing data contributed by over 20,000 women with PCOS (“cysters”) worldwide, StuffThatWorks is aiming to discover why there’s still so much mystery around this common condition and provide insights on why so many women are being misdiagnosed.
How is PCOS diagnosed?
There are multiple versions of PCOS diagnostic criteria, yet the most common is high androgen levels (hyperandrogenism) in the blood with irregular ovulation and/or the presence of “pearl-like” cysts on the ovaries determined by ultrasound. Symptoms of high androgens are acne, thinning scalp hair, and excessive facial or body hair.
Sadly, but not surprisingly, the majority of PCOS patients start experiencing symptoms at the onset of puberty, but are dismissed as being part of adolescence; only to discover they have PCOS much later in life, typically when they have trouble conceiving, or are diagnosed with another metabolic condition like diabetes, which affects up to 50% of women with PCOS before they reach the age of 40.
In our next blog post, we’ll show that excessive facial or body hair, also known as hirsutism, is “the most indicative symptom of PCOS” (What exactly does that mean? Stay tuned for our next post!). Indicating it’s value as a significant warning sign of PCOS and something definitely worth mentioning to the doctor along with any other symptoms.
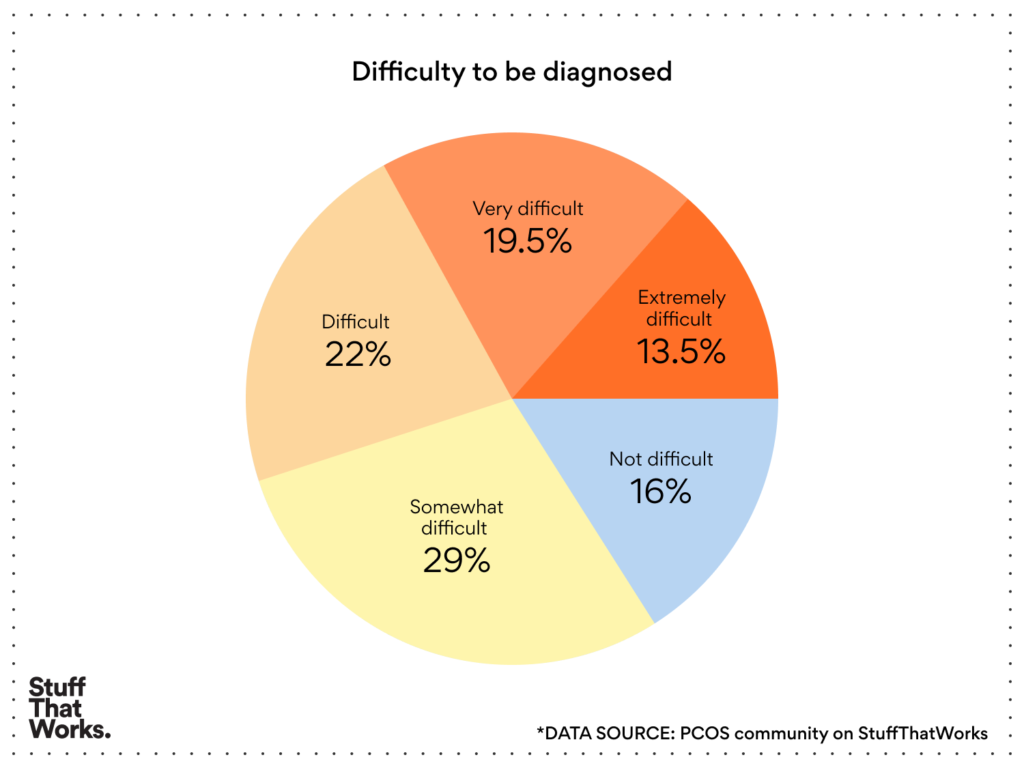
More than a third of women with PCOS find it very to extremely difficult to be diagnosed:
Does the type of doctor you see make a difference?
While the natural inclination may be to schedule an appointment with a gynecologist or family doctor, one of the primary means of diagnosis, the androgen level test, is actually one of an endocrinological nature. According to the analysis of StuffThatWorks data, the members of the PCOS community who reported it was “easy” to be diagnosed, were women that had a higher prevalence of endocrinological conditions such as hypothyroidism, hyperthyroidism, and diabetes is, which implies they actually saw an endocrinologist, either prior to or after their PCOS diagnosis. So if you’re struggling to be diagnosed, perhaps a visit to an endocrinologist can lead you in the right direction.
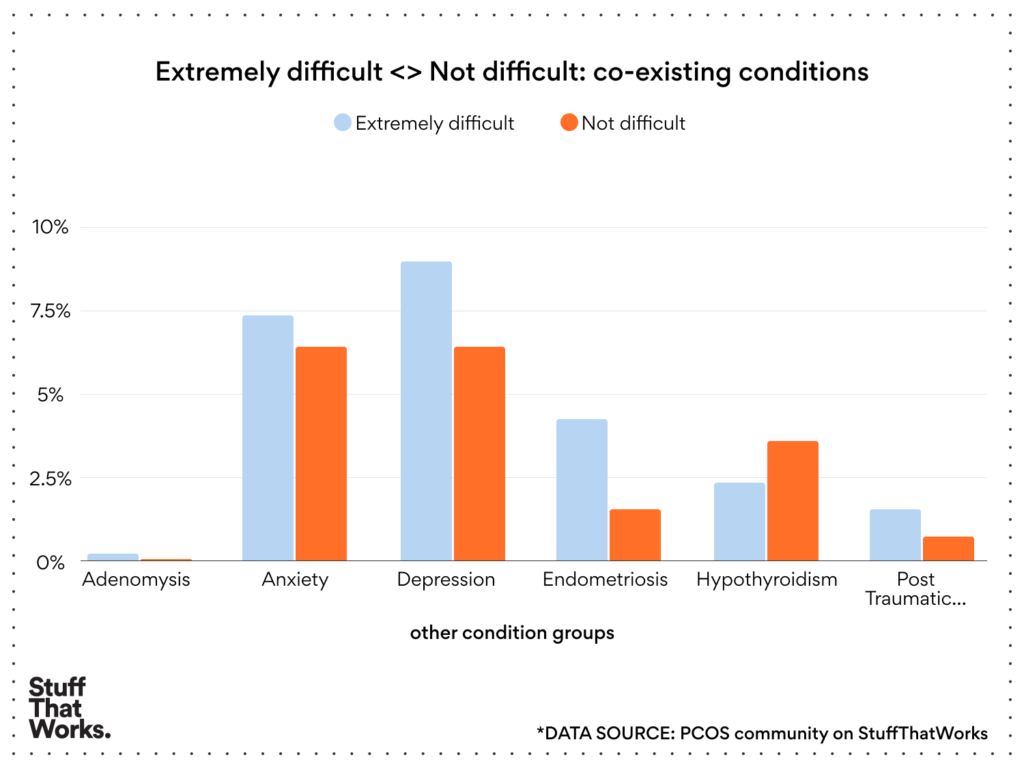
Does having other conditions make being diagnosed with PCOS more challenging?
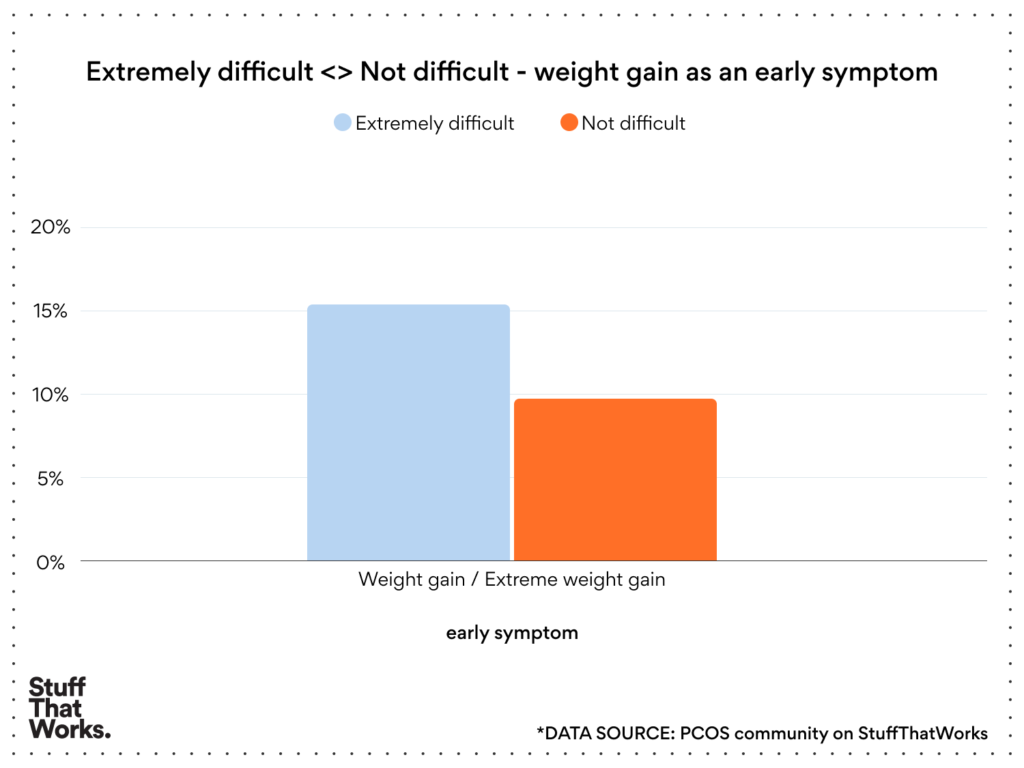
Members of the PCOS community who reported their diagnosis process as extremely difficult had a higher prevalence of three specific types of conditions: gynecological conditions such as endometriosis and adenomyosis; obesity or being overweight (an early and significant symptom of PCOS for some women); and mental health conditions such as depression, anxiety, and PTSD. This might indicate that the existing conditions were linked to their PCOS, a distraction to the diagnosis, or that the delayed diagnosis and lack of validation caused real physical and mental harm.
Women suffering from depression, anxiety, and endometriosis have the hardest time being diagnosed
Women who experienced “extreme difficulty” being diagnosed with PCOS suffered 50% more from “extreme weight gain” as an early symptom than those who were “easily” diagnosed
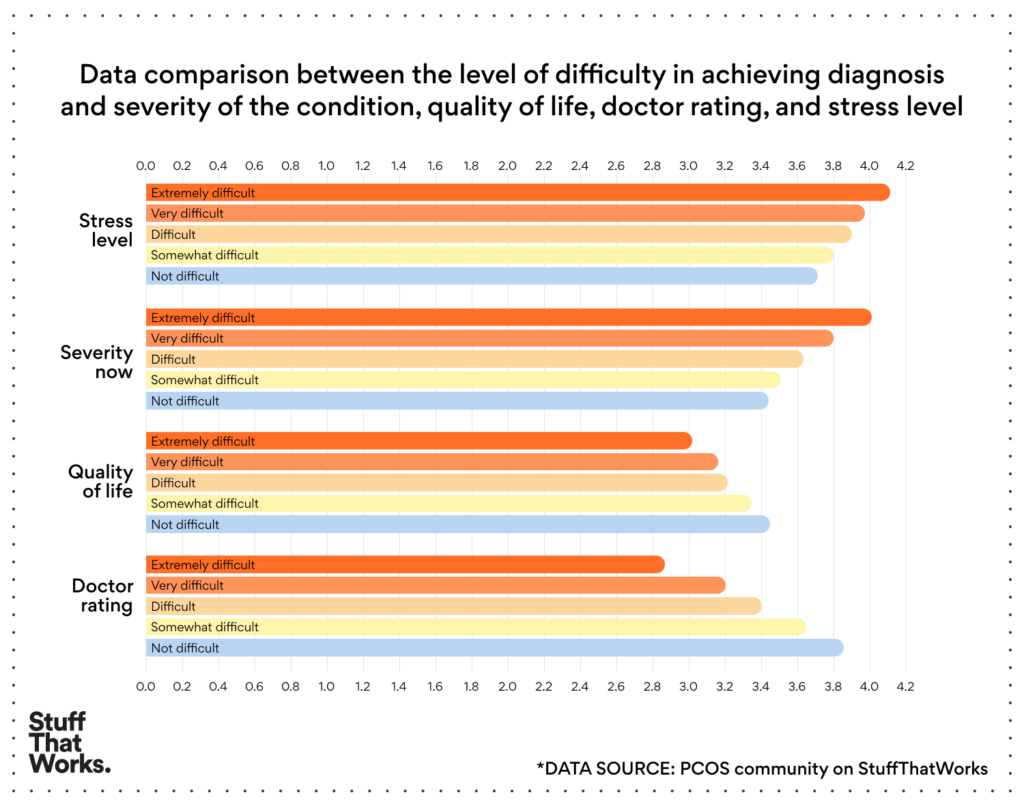
Being satisfied with your doctor is good for your health, and vice versa.
Unsurprisingly, our data insights indicate that the level of patient-physician satisfaction and quality of life progressively decline as the diagnosis process increases in difficulty and the severity of the condition worsens. External research reinforces that the level of dissatisfaction is so significant that physician education to identify the gaps in PCOS knowledge and practice patterns is critical to improving the quality of treatment experience and satisfaction regarding diagnosis. Inconsistent approaches related to diagnosis and treatment have resulted in frustration and lack of faith in physicians among women being diagnosed with and treated for PCOS.
It’s never too late to take your health in your own hands.
While there is no cure for PCOS yet, there are ways to effectively manage the condition and lifestyle changes that can make a major difference. But in order to make these changes, women need to be aware that they have the condition. Far too often PCOS is discovered once a woman has made the decision to become pregnant and experiences difficulty conceiving naturally; a shattering time to receive a diagnosis that your fertility could be compromised. Others discover they have PCOS only when a secondary disorder or disease is discovered. PCOS causes a myriad of symptoms and serious health problems that can affect a woman’s mental, physical, and reproductive health – and a missed diagnosis and possibly misdiagnosis and lack of validation only worsen her wellbeing and outlook.
For all the evidence listed above and the countless stories of women whose symptoms like acne, hirsutism, and weight gain were overlooked and dismissed, while the real root of the problem went untreated and unaddressed, it is painfully clear that PCOS awareness is greatly lacking and is critical for every woman. Know the signs, know the tests to ask for, follow your gut, and be your own best advocate. Recognizing the early symptoms of PCOS puts the power in women’s hands to best manage their symptoms and protect their fertility for the future. Let’s close the gaps in education and support for women with PCOS.
- Thanks very much, @Deanna Siegfried and @Yoav Litani for your insights and help with this blog post.
If you or someone you love has PCOS, join the PCOS community on StuffThatWorks.